Published date: 2025-06-19 Last updated: 2025-12-19
Patient monitoring refers to the continuous tracking of a patient's vital signs using professional medical equipment. The primary goals are to closely monitor the patient's health status in real time, detect abnormalities at an early stage, and accelerate medical response. This system is widely applied in Intensive Care Units (ICUs), operating rooms, emergency departments, and more recently, in the rapidly growing fields of telehealth and home care.
In clinical scenarios where patient safety is the top priority, patient monitoring serves as a critical nexus connecting artificial intelligence, medical cloud platforms, wearable devices, and predictive diagnostics. By automating and collecting physiological data efficiently, healthcare professionals(HCPs) can promptly detect changes in patient conditions and deliver more personalized and responsive treatments.
Patient monitors are medical devices designed to simultaneously track multiple physiological parameters. Based on usage scenarios and functionality, these devices can be categorized as follows:
Most of these traditional devices require integration with SaMD to enable functions such as data analysis, interpretation, and predictive alerts.
For further reading:FaceHeart’s Perspective: Chronic Disease Management with Remote Monitoring
Unlike traditional monitors, FaceHeart Vitals™, a video-based vital sign solution, requires no physical contact or wearable device. Instead, it leverages a regular camera to scan a person's face for 50 seconds and provides readings of the following indicators:
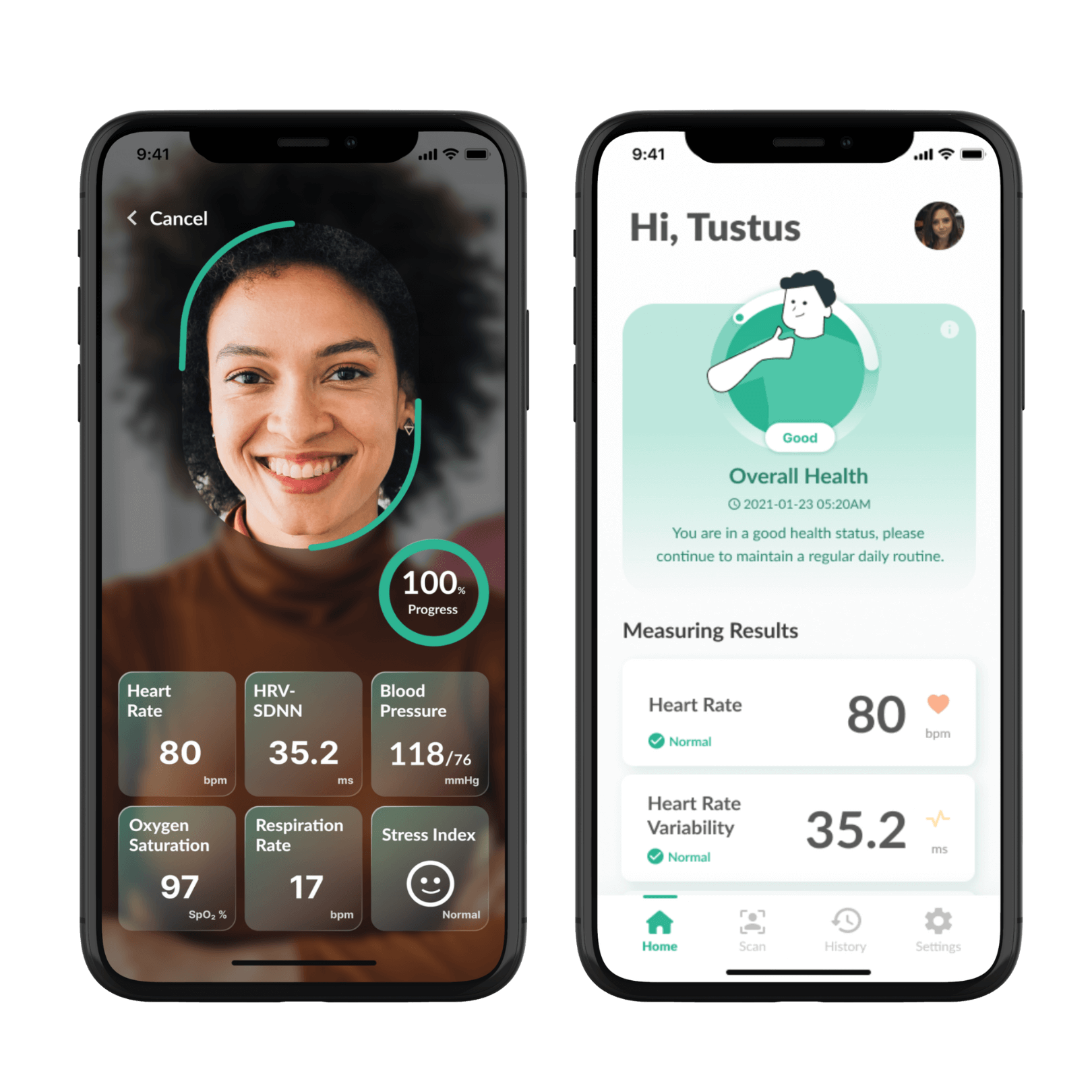
The core technology, remote photoplethysmography (rPPG), extracts subtle color changes under the human facial tissue through reflected ambient light captured by the camera, enabling fully contactless measurement. Current applications include elderly care monitoring and risk assessment in the finance and insurance sectors.
Key Advantages:
Across all medical contexts, the five vital signs serve as critical indicators for assessing patients’ current condition and long-term health trends. Below is a detailed overview of their clinical relevance and use cases:
Heart rate refers to the number of times the heart contracts per minute and is a key indicator of cardiovascular activity. Abnormalities such as tachycardia (fast heart rate, HR >100 bpm) or bradycardia (slow heart rate, HR <60 bpm) may signal arrhythmias, shock, or adverse drug effects. Continuous heart rate monitoring enables early detection of acute events such as atrial fibrillation and also provides data for AI-driven cardiovascular risk assessment.
Blood pressure reflects the force exerted by circulating blood on arterial walls, serving as an indicator of circulatory load and vascular elasticity. When elevated, this pressure–known as hypertension–is closely linked to stroke and kidney disease, while hypotension may suggest internal bleeding or sepsis. Smart blood pressure monitors can automatically track trends, helping patients manage their condition more effectively.
SpO₂ represents the percentage of oxygen-saturated hemoglobin in the blood. Readings below 92% typically indicate respiratory impairment, such as chronic obstructive pulmonary disease (COPD) or COVID-19. Wearable SpO₂ sensors combined with telehealth platforms can deliver real-time alerts for hypoxia risk.
Temperature is a vital indicator of immune response and metabolic activity. Fever is a common sign of infection or inflammation, while hypothermia may occur in septic shock or post-operative complications. Smart thermometers integrated with AI analytics help monitor chronic inflammatory conditions over time.
Respiratory rate is influenced by the central nervous system, metabolic imbalances, emotional states, and cardiopulmonary diseases. Once difficult to track, new technologies such as non-contact imaging analysis and chest strap sensors provide accurate measurements. These are especially valuable for detecting obstructive sleep apnea (OSA), post-COVID symptoms, and in emergency triage settings.
Deploying smart patient monitoring systems not only enhances the quality of medical care but also streamlines care delivery. The following outlines five tangible benefits:
During sudden shifts in health condition—such as a rapid drop in blood pressure or irregular heart rhythms—the system can trigger visual and auditory alarms within seconds, enabling clinical staff to respond immediately and effectively.
Automated data collection and logging reduce the risk of transcription errors while also ensuring higher data integrity and better traceability of patient records.
Continuous monitoring is particularly beneficial for elderly patients and those with conditions such as diabetes or heart disease. By detecting health deterioration early, it contributes to lower emergency room utilization and fewer hospital readmissions.
By integrating wearable devices with mobile apps, patients in remote or underserved regions can transmit their vital signs report to medical teams in real time, bridging gaps in access to healthcare.
Longitudinal physiological data contributes to building individual health baselines, facilitating the development of precision medicine and predictive diagnostics powered by AI models.
These devices represent the current advancements in medical technology and applications, addressing the growing demand for both clinical care and remote monitoring.
| Device Name | Functions & Advantages | Application Scenarios |
|---|---|---|
| Continuous Glucose Monitor (CGM) | Real-time tracking of blood glucose changes; supports remote alerting and personalized settings | Diabetes management, post-operative glucose control |
| AI-Based ECG Analysis Platform | Automated arrhythmia detection; enhances efficiency and accuracy of cardiac diagnostics | Home care, cardiac risk screening, community clinics |
| Portable Ultrasound (POCUS) | Handheld and mobile; image quality suitable for point-of-care diagnostics | Emergency, rural medical visits, military healthcare |
| Remote Multi-Parameter Monitoring Platform | Continuous monitoring of SpO₂, BP, HR, RR, etc. | Home care, assisted living centers, corporate health programs |
For further reading:Complete Guide to SaMD: Definition, Regulations, and Future Trends
According to reports from the FDA and industry analyses, 2025 is expected to signal a major breakthrough in the integration of software and hardware medical technologies, particularly in the following areas:
The use of AI-powered image analysis systems is rapidly expanding in clinical and remote healthcare settings to monitor physiological parameters in a contactless and real-time manner, giving continuous health insights with minimal user input.
Reference:
FDA Emergency Use Authorization (EUA) list for Remote Monitoring Devices
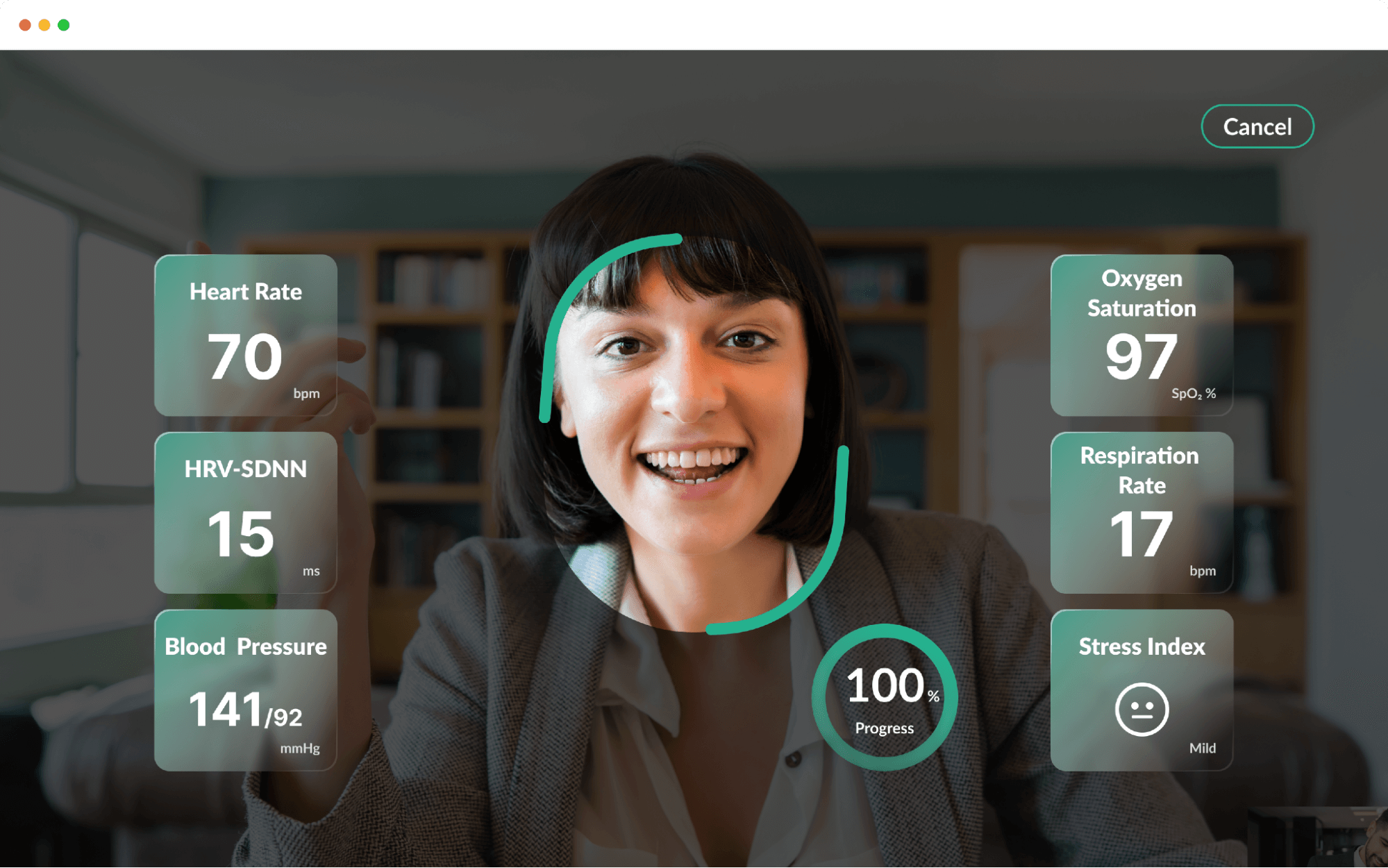
Amid the growing demand for non-contact health monitoring, FaceHeart Vitals™ has emerged as a global innovation leading product in the field of Remote Patient Monitoring (RPM). Developed by FaceHeart, the solution is powered by the cutting-edge rPPG technology, which uses standard cameras to analyze subtle skin color changes on the user's face—without the need for any wearable device.
Within just 50 seconds, FaceHeart Vitals™ can accurately provide the following vital signs:
FaceHeart Vitals™ is the first AI-based medical software in the world to be granted by FDA as a Class II SaMD for heart rate and respiratory rate monitoring using only a standard camera— marking a major breakthrough in the regulatory approval of contactless vital sign measurement technologies.
So far, FaceHeart has conducted clinical validations on over 6,000 participants in collaboration with leading medical institutions such as National Taiwan University Hospital (NTUH), Chang Gung Memorial Hospital, and Taichung Veterans General Hospital, as well as with medical providers in the United States. The system has accumulated over 300 million physiological data points.
Data source: GbiMonthly News Report
FaceHeart Vitals™ has been successfully deployed in a wide range of settings:
Its non-invasive, contactless design makes it especially well-suited for home settings, long-term care, and post-pandemic high-efficiency healthcare delivery, meeting the growing need for user-friendly, comfort-focused patient monitoring solutions.
| Dimension | Focus | Advantage Description |
|---|---|---|
| Core Technology | rPPG | Contactless, no need of devices, enables diverse and scalable deployment |
| Regulatory | FDA Class II SaMD | Certified for use in international medical markets |
| System Integration | API/SDK + EMR connectivity | Easily integrates into cloud ecosystems and electronic medical records |
| Application Scenarios | Hospitals, homes, enterprises, rural areas | Seamless adaptation across all environments; scalable with low deployment costs |