Published date: 2025-12-10 Last updated: 2026-01-27

Globally, chronic diseases are the primary cause of morbidity and account for 71% of all mortality, with approximately 25% of adults suffering from one or more persistent health issues.[1] AS these conditions rise and populations age, placing a significant strain on healthcare infrastructures, smart home healthcare has become a critical, cost-effective direction for modern systems.
Smart home healthcare is a transformative model in modern healthcare that integrates Internet of Things (IoT), Artificial Intelligence (AI), and cloud computing into the home environment to shift focus from hospital-centric to patient-centered care. It has allowed for the continuous, real-time monitoring of vital signs and behavioral patterns. [2] By combining connected sensors, cloud platforms, and the use of AI in healthcare, health monitoring can move beyond hospitals and clinics into everyday living environments. These intelligent environments support independent living and enable the early detection of health deterioration, which helps reduce hospital occupancy and improves the quality of life for vulnerable populations. [3]
Smart home healthcare integrates advanced technologies like the Internet of Things (IoT), Artificial Intelligence (AI), and cloud computing into the residential environment to shift the focus from hospital-centric to proactive, patient-centered care to the home environment. Connected devices continuously collect physiological and behavioral data, send data to the cloud and medical teams, and support early detection of potential health issues, reducing unnecessary hospital visits.
This foundational layer is responsible for the continuous and passive collection of health and behavioral data. It includes wearable devices such as smartwatches, ECG monitors, and continuous glucose monitors to track vital signs [4]. Common examples include blood pressure monitors, blood glucose meters, weighing scales, smartwatches, and sleep rings, which have already helped millions of people track essential health metrics at home.
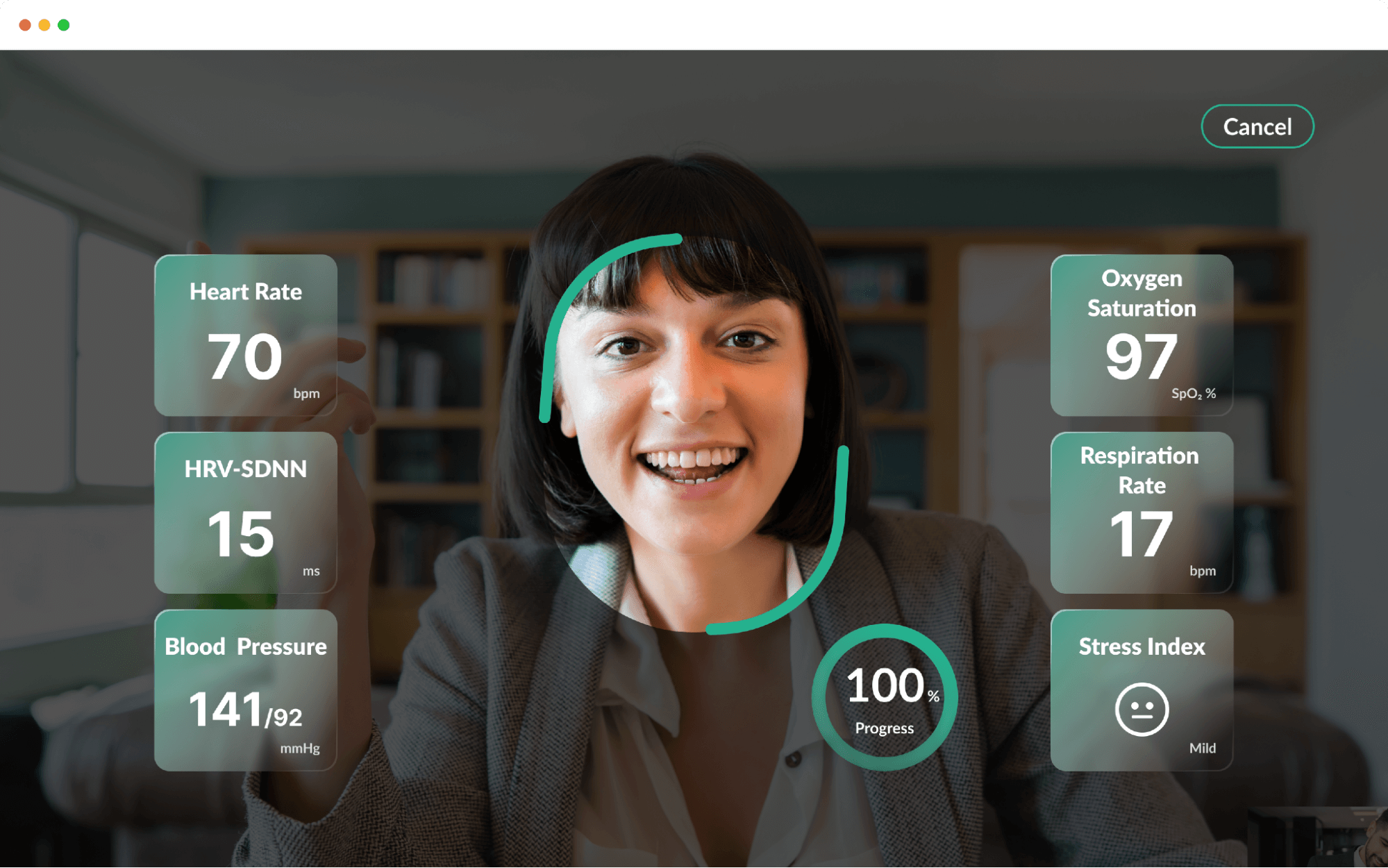
As smart home ecosystems evolve, more advanced solutions are being introduced, including activity and fall detection sensors, in-home monitoring cameras, and emerging contactless vital signs monitoring technologies. By using an ordinary camera combined with AI-based analysis, these solutions can estimate heart rate, respiratory rate, and blood pressure trends without requiring users to wear any additional devices, significantly improving comfort and long-term usability.
Devices such as smart speakers , a home control panel, or even your Wi-Fi router often serve as central hubs in a smart home health care system. These are often complemented by ambient sensors that collect data non-intrusively, including passive infrared (PIR) motion detectors, smart weighing scales, and bed scales capable of measuring weight, respiratory rates, and ballistocardiograph (BCG) energy while the patient sleeps. These devices collect data from all connected sensors, perform initial processing or assessments, and determine which information should be uploaded to the cloud and which can be processed locally at home. This ensures faster responses, reduced bandwidth usage, and improved data security.
Cloud platforms and databases serve as the backbone of a smart home health care system, providing a centralized environment for storing and managing the massive volumes of data generated by IoT devices. They securely store long-term health data, generate trend visualizations, and use AI or ruled-based analytics to analyze patterns. These cloud-based systems ensure that health information is accessible anytime and anywhere, allowing for real-time data sharing between patients, researchers, and healthcare specialists across different geographic boundaries.
When a smart home health system is integrated into a hospital, clinic, or long-term care provider, clinicians are able to review patients' recent and historical data before appointments. These services facilitate remote patient monitoring (RPM), allowing clinicians to track vital signs such as heart rate, blood pressure, and blood glucose levels in real-time, which shifts care from traditional hospital-centered models to patient-centric environments. This gives clinicians a better picture of patients’ condition over time and supports more evidence-based decisions . On top of that, telehealth and telemedicine remove geographic barriers by offering virtual consultations and diagnostic services directly to the home, which is especially beneficial for managing chronic diseases and supporting individuals with disabilities. In elder care settings, subtle changes in vital signs readings or other daily behavior can be detected early, allowing caregivers to intervene before conditions escalate.
The current state of artificial intelligence (AI) in healthcare is characterized by a rapid paradigm shift from traditional, reactive models to proactive, personalized, and patient-centered care. By integrating with the Internet of Things (IoT) and the Internet of Medical Things (IoMT), AI has revolutionized Remote Patient Monitoring (RPM), allowing for the continuous collection and analysis of physiological data outside of clinical environments [5]. Machine learning and large-scale data analytics enable rapid processing of complex medical data, supporting disease assessment, risk prediction, and care planning.
Beyond monitoring, AI is increasingly employed in Clinical Decision Support Systems (CDSS) to assist healthcare providers in diagnosing diseases like cancer with high precision and in managing chronic illnesses through tailored treatment plans. From an operational perspective, AI supports patient triage, resource allocation, and workflow optimization in care. As home-based care expands , the use of AI in healthcare has extended into smart home health care, enabling continuous, non-invasive monitoring outside traditional clinical environments.
Overall, AI is driving a shift from a reactive, treatment-focused model to a proactive approach centered on prevention and risk management. This transformation reduces the burden on healthcare systems while empowering individuals to take a more active role in managing their health. Despite this progress, the field faces ongoing challenges, including the need for AI explainability to gain clinical trust, the high cost of initial infrastructure, and stringent requirements for data security and regulatory compliance.
As lifestyles continue to change, chronic conditions such as cardiovascular disease, diabetes, and hypertension require continuous management rather than episodic treatment. Traditional reactive models focused on hospital-centered care are becoming unsustainable as chronic diseases remain the leading cause of morbidity and mortality globally. Smart home healthcare shifts the focus to proactive and patient-centered care, extending medical support into residential environments to manage long-term conditions.
By combining smart home monitoring with AI-driven analytics , long-term health trends and subtle changes can be identified earlier, enabling proactive intervention and more effective chronic disease management.
Population aging has become a global structural challenge. Traditional care models that rely heavily on hospitals and institutional facilities are no longer sufficient to meet future demand. Smart home healthcare empowers the elderly and individuals with chronic illnesses to maintain their independence in a familiar environment, a concept known as aging-in-place [6]. Smart home health helps to maintain independence, dignity, and quality of life for the elderly while alleviating pressure on healthcare and long-term care systems.
Many serious health conditions typically develop gradually rather than appearing suddenly. However, traditional medical checkups fail to identify these conditions early because they rely on intermittent measurements and manual records that are limited by clinical workload and resource availability. . Smart home health care addresses this gap by providing frequent, long-term, and low-friction monitoring within daily life. Advanced AI-driven analysis—employing models such as LSTM and CNN—interprets these complex data streams to recognize patterns and issue early warning alerts [8].
In smart home health care, artificial intelligence is not a standalone technology but a multi-layered system that integrates digital tools to shift medical models from reactive care to proactive, personalized, and preventive care. This ecosystem relies on a sophisticated architecture that coordinates data collection, intelligent analysis, and clinical delivery to provide real value to patients and providers. From front-end health data collection to AI-driven analysis and the integration of medical and care services, each layer plays a critical role. The following sections outline the core AI architecture behind smart home health care, illustrating how AI in healthcare is translated into practical, everyday applications.
The foundation of SHC is the Internet of Medical Things (IoMT), which utilizes a network of connected devices and sensors to continuously capture physiological and behavioral data. Technologies at this layer include wearable devices, non-invasive sensors, imaging systems, and audio-based sensing equipment. These tools measure vital signs, activity levels, and daily behaviors.
The data analytics and AI layer represents the core value of AI in healthcare, employing advanced algorithms to interpret the massive volumes of data stored in cloud, fog, or edge platforms. This layer analyzes long-term health data to identify personalized health patterns and potential risks.
Rather than relying on single measurements, AI focuses on trends and changes over time, to identify physiological shifts or behavioral changes, enabling predictive and proactive health monitoring. For example, Convolutional Neural Networks (CNN) are used to classify complex patterns, such as identifying falls or detecting cardiac arrhythmia and respiratory distress.
The final layer translates AI insights into practical clinical outcomes through Remote Patient Monitoring (RPM) and Clinical Decision Support Systems (CDSS). . They can both be integrated into hospital information systems (HIS), clinic electronic medical records (EMR), long-term care platforms, and corporate health management systems. Through this integration, analytical results are delivered as alerts, reports, care recommendations, or follow-up workflows.
Through well-designed service workflows, smart home health care goes beyond simply providing data and becomes a practical tool that actively supports health management and care decision-making. AI can identify early signs of health deterioration—such as sepsis, heart attacks, or diabetic episodes—up to an hour before they present clinically [9]. This approach creates an efficient loop where information flows from sensors to AI for insight, returning as targeted medical interventions that reduce hospital occupancy and improve the quality of life for vulnerable populations. .
 As the healthcare industry shifts toward proactive, personalized care, the rise of smart home health ecosystems has introduced unprecedented convenience for chronic disease management. However, the integration of Ai in healthcare requires the continuous collection of massive volumes of sensitive physiological data, leading to urgent questions about whether this information is truly secure. While these technologies offer life-saving potential, they also present significant vulnerabilities that must be addressed through advanced architectural and technical safeguards.
As the healthcare industry shifts toward proactive, personalized care, the rise of smart home health ecosystems has introduced unprecedented convenience for chronic disease management. However, the integration of Ai in healthcare requires the continuous collection of massive volumes of sensitive physiological data, leading to urgent questions about whether this information is truly secure. While these technologies offer life-saving potential, they also present significant vulnerabilities that must be addressed through advanced architectural and technical safeguards.
The evolution of smart home health represents a significant paradigm shift toward proactive, patient-centered care, yet it remains one of the most sensitive scenarios within the Internet of Things (IoT) because it involves the continuous collection of deeply personal medical records and real-time physiological data. A typical home environment includes numerous connected devices from different manufacturers, operating under inconsistent security standards and update cycles. Furthermore, unlike general consumer IoT applications, the integration of Ai in healthcare introduces a complex layer of risk associated with personally identifiable information, data rights, and stringent ethical considerations.
When smart home devices begin collecting and processing sensitive health data, such as physiological signals, daily behaviors, and long-term health trends, the potential impact of data breaches or misuse increases significantly. Maintaining high standards for data privacy and cybersecurity is critical to the successful deployment of these technologies, ensuring that vulnerable populations can safely benefit from independent living and "aging-in-place." As a result, smart home health care is widely regarded as one of the most security-critical use cases within the broader Internet of Things (IoT) landscape.
In response to the rapid growth of smart devices and AI-driven healthcare technologies, regulatory authorities are increasingly establishing formal safeguards to protect users’ data and privacy.
To ensure the security of sensitive medical information in smart home health ecosystems, both users and organizations must adopt proactive technical and behavioral strategies. Regulatory labels and official privacy guidelines provide a practical framework for evaluating smart home health care solutions. In addition, users can safeguard their privacy by participating in digital literacy training to effectively manage their Personal Health Records via secure eHealth portals and mobile applications. Prioritizing products that carry third-party security certifications, follow privacy-by-design principles, or clearly disclose how data is collected, stored, and used can significantly reduce exposure to high-risk devices.
Organizations are responsible for establishing a robust ethical and technical framework by strictly adhering to international data protection regulations like GDPR and HIPAA. Fostering interdisciplinary collaboration between technology experts and healthcare professionals ensures that privacy protocols are clinically relevant and ethically governed.
For both users and healthcare providers, certifications and compliance with recognized standards provide a reliable first point of reference when evaluating smart health technologies.
Against this backdrop, let’s take a closer look at the challenges FaceHeart is designed to address in smart home health care.
FaceHeart adopts an SDK-based approach rather than relying on proprietary, closed hardware devices. FH Vitals SDK enables existing devices, such as computers, smartphones, and tablets, to perform contactless vital signs monitoring using only a screen and a standard camera. This transforms daily devices to health care tools which significantly reduces deployment costs and improves overall user acceptance.
FaceHeart leverages Remote Photoplethysmography (rPPG) to capture subtle facial color changes via standard camera. These signals are reconstructed into pulse waveforms to estimate key health indicators such as heart rate.
From the user’s perspective, the process is simple: open the app or camera, sit still, face the camera for approximately 50 seconds, and complete a full physiological measurement.
Data security and privacy protection are central to FaceHeart’s system design, reflecting the high level of trust required in smart home health care. FaceHeart processes physiological signals in real time without storing any facial images or performing facial recognition. All data conversion and deletion are performed locally, and no facial recognition or identity matching is conducted.
This privacy-first approach enables health measurements while minimizing personal data exposure and aligning with international data protection regulations such as GDPR and HIPAA, providing a trusted foundation for AI applications in healthcare. These regulatory frameworks ensure that the continuous collection of sensitive physiological data is handled with the highest level of security and accountability.
The software has received U.S. FDA 510(k) clearance as a Software as a Medical Device (SaMD), enabling contactless measurements using a standard camera. The cleared solution includes measurement modules for key physiological parameters, such as respiratory rate. Receiving FDA clearance not only represents the recognition of FaceHeart’s undivided attention to clinical trials, but also reinforces its commitment to deliver accessible and reliable contactless vital sign measurement to the general public.
For more information on FaceHeart technology, devices, applications, and a live demo, contact [email protected]
FaceHeart opens up practical, meaningful use cases for smart home health monitoring. Here is a look at a few scenarios:
All of these scenarios share one important feature: you don’t need any extra medical devices. A camera and screen that people already use every day are sufficient to deliver medical-grade, continuous health monitoring at home.
Smart home health care shifts routine monitoring and follow-up care from hospitals and care facilities into the home, as real-time analysis with RPM technology can identify health deterioration before it becomes critical, thereby slashing emergency room visits and hospital admissions. By enabling continuous, remote health monitoring, healthcare providers can focus limited medical resources more effectively toward acute and high-risk cases. This approach improves the overall efficiency and sustainability of healthcare and long-term care systems. By leveraging AI in healthcare for continuous monitoring, these systems alleviate the burden on an overwhelmed healthcare system and directly address critical workforce shortages by reducing the need for manual oversight.
By delivering health monitoring and care support in familiar living environments, smart home health care promotes independence, dignity, and peace of mind for older adults. Furthermore, smart home technology fosters a more inclusive and equitable society by providing high-quality care to individuals with disabilities who face challenges traveling to clinical facilities. Seniors can maintain daily routines while caregivers and medical teams stay informed of health changes, enhancing quality of life while reducing reliance on institutional care. Ultimately, by integrating objective, real-time data with clinical practice, smart home health care not only improves the quality of life for vulnerable elderly populations but also builds public confidence in the sustainability of modern healthcare systems.
Continuous monitoring and early risk detection enable timely intervention before health issues escalate into costly medical events. The primary driver of cost reduction is the ability of AI-enabled Remote Patient Monitoring (RPM) to detect signs of health deterioration before they reach a critical state. By preventing unnecessary emergency visits, hospitalizations, and complications, smart home health care significantly reduces avoidable healthcare spending at individual and system levels. Case studies involving AI-augmented monitoring have demonstrated a 15% reduction in average healthcare costs, saving approximately $1,500 per patient by replacing high-cost emergency care with continuous home management.
By fostering an ecosystem of continuous monitoring and early detection, smart home health care not only improves the quality of life for vulnerable populations but also provides a sustainable solution to the global healthcare cost crisis.
AI will continue to enhance telemedicine by providing real-time decision support, automated triage, and continuous patient monitoring. This synergy, often categorized under "smart healthcare" (SHC), extends medical services beyond physical facility boundaries into homes and workplaces, ensuring continuous connectivity between patients and providers. The deep integration of AI into telemedicine transforms a static video consultation into a dynamic intelligence ecosystem, enabling more responsive, data-driven remote care.
As AI models learn from long-term individual health data, the personalized health risk prediction will become more accurate and actionable. Modern models have matured to achieve accuracy levels between 93% and 97% in detecting early signs of health deterioration—including heart attacks, diabetic episodes, and sepsis—often before clinical symptoms are even present. This supports earlier and more targeted preventive interventions tailored to each individual.
The widespread adoption of contactless health monitoring represents a fundamental transition from invasive, skin-contact devices to noninvasive, digital technologies that enable continuous tracking without disrupting a patient’s daily routine. Camera- and sensor-based systems reduce friction in daily health monitoring while increasing long-term user engagement.
Stronger interoperability standards will improve data exchange between hospitals, clinics, and home care systems. Systems should align with internationally recognized data and messaging standards to ensure that information flows are reliable from day one. This standardization will enable seamless and coordinated care across the entire care continuum.
As AI-driven healthcare solutions mature, governments and regulatory bodies will establish clearer rules around transparency, accountability, and data protection. These frameworks will play a critical role in strengthening trust and supporting responsible adoption.
Smart home health care is well suited for the elderly, individuals with chronic conditions, caregivers, and anyone interested in proactive lifestyle health management at home. Solutions like FaceHeart Vitals™ are particularly valuable for users who prefer low-friction, contactless monitoring, enabling them to perform regular health checks using devices they already own, such as smartphones, tablets, or laptops.
When developed and validated under medical device standards, AI-based health monitoring can deliver reliable and clinically meaningful insights. FaceHeart Vitals™, for example, has received two U.S. FDA 510(k) clearance under Class II Software as a Medical Device (SaMD), indicating that its contactless measurements, including heart rate and respiratory rate,meet regulatory requirements for safety and effectiveness. The solution is designed to monitor health trends and support clinical decision-making, rather than replacing diagnostic tools.
No. Smart home health care solutions, including FaceHeart Vitals™, are designed to support existing healthcare professionals rather than replace them. By capturing health data regularly over time, these tools give HCPs better visibility into patients’ long-term health trends, enabling more informed and timely medical decisions.
Not necessarily. When FaceHeart Vitals™ is integrated as one of the smart home system’s features, it can work with regular cameras on existing devices such as smartphones, tablets, and computers. This allows users to monitor their health without purchasing additional bulky medical hardware at home, helping reduce overall costs.
Data security and privacy are critical in smart home healthcare. FaceHeart Vitals™ is built with privacy-by-design principles: physiological data is processed locally on the user’s device, without sending raw data to external servers. All the data are owned by the user and facial images are discarded when the measurement is completed. This approach aligns with international data protection practices, helping minimize privacy risks while enabling health monitoring.
For more information on FaceHeart technology, devices, applications, and a live demo, contact [email protected]
Disclaimer: FaceHeart Vitals™ is not intended for diagnostic purposes. If you have any health concerns, please consult your healthcare provider.