Published date: 2025-08-11 Last updated: 2026-01-28
As healthcare shifts toward patient-centered and preventive models, remote patient monitoring (RPM) devices have become a critical foundation of modern telehealth. Advances ranging from wearable technologies to Contactless Vital Sign Measurement enable continuous, non-invasive monitoring beyond traditional clinical environments. This article explores the evolution, applications, and future trends of remote patient monitoring devices, while introducing FaceHeart, an innovative contactless vital sign measurement solution revolutionizing the next generation of digital healthcare.

Remote patient monitoring (RPM) devices are digital health tools that enable healthcare professionals to collect patients’ physiological data either continuously or at regular intervals. The key benefit brought by RPM is that it can be conducted without the need of in-person visits.
These devices play a crucial role in chronic disease management, supporting conditions such as cardiovascular disease, diabetes, and asthma. For patients with these chronic diseases, vital signs monitoring are essential for health professionals to detect abnormalities promptly. Over time, the scope of remote patient monitoring has expanded to cover acute illness care, oncology, sleep disorders, and even maternal health monitoring.
A wide range of remote patient monitoring devices are commonly in use today, including:
While some of these devices are integrated into hospital systems, many are designed for home-based use, enabling patients to take an active role in managing their health. Home-based designs are also beneficial for patients with mild symptoms who wish to stay at home. Most RPM devices can seamlessly transmit physiological data to secure medical platforms, allowing healthcare providers to assess trends, detect anomalies, and make timely clinical interventions.
Further Reading:What Is Remote Vital Signs Monitoring? Comprehensive Health Monitoring Insights!

According to the U.S. Centers for Disease Control and Prevention (CDC), remote monitoring supports proactive care models by helping clinicians identify health risks before they escalate. The U.S. Food and Drug Administration (FDA) also recognizes RPM technologies as essential tools for expanding access to care while maintaining clinical oversight.
Below are five of the most commonly used remote patient monitoring devices in today’s healthcare environment:
Remote blood pressure monitors are widely used to manage hypertension and cardiovascular conditions. These devices automatically record blood pressure readings and securely transmit the data to healthcare platforms, allowing clinicians to monitor trends over time and adjust treatment plans remotely.
Heart rate monitors and multi-parameter vital signs monitoring devices track key physiological indicators such as heart rate, respiratory rate, and sometimes oxygen saturation. These tools are especially valuable for people with heart conditions, patients recovering from surgery, or individuals living with chronic health issues.
Connected blood glucometers enable patients with diabetes to measure and upload their blood glucose levels at home and share the results with their caregivers or health professionals. Having access to continuous data helps improve glycemic control and allows healthcare providers to identify potential risks or abnormal patterns at an earlier stage.
Smart weight scales are commonly used in heart failure and chronic disease management programs. By tracking changes in a patient’s weight over time, these devices help healthcare providers detect early signs of fluid retention and intervene before symptoms worsen.
Respiratory monitoring devices, including apnea detection sensors, help track breathing patterns and sleep-related conditions. These devices are often used for patients with sleep apnea, chronic obstructive pulmonary disease (COPD), and other respiratory disorders.
Together, these remote patient monitoring devices enable a more proactive, data-driven approach to care that extends far beyond the clinic. Research shows that RPM can help reduce hospital readmissions, emergency department visits, and other costly acute care use by detecting health issues early and supporting timely clinical intervention. For patients with chronic conditions or those discharged after hospitalization, home telemonitoring has been associated with significant reductions in hospitalizations and total hospital days at both 3 and 6 months after implementation.
By advancing care continuity, patient engagement, and early risk detection, RPM supports long‑term health management, enhances clinical outcomes, and contributes to cost‑effective healthcare delivery.
In recent years, innovations in sensor technology and AI have driven the evolution of RPM devices from traditional wearable systems to fully Contactless Vital Sign Measurement technologies. This next-generation approach uses imaging, radar, and optical techniques to measure vital signs without the need for physical contact, electrodes, or wearable patches, enabling more convenient and comfortable monitoring for patients and caregivers alike
Contactless Vital Sign Measurement refers to the ability to monitor physiological parameters such as heart rate, respiratory rate, blood pressure, and oxygen saturation without directly touching the patient’s skin. These technologies offer significant advantages in comfort, hygiene, and scalability—especially for sensitive or vulnerable populations such as underserved areas, undeserved areas that has limited hospital facilities with access to constant health condition checks.
Contactless Vital Sign Measurement offers a non-invasive approach that eliminates physical discomfort from patches and frictions associated with wearable devices. By removing additional devices attached to the patients, this technology significantly reduces the risk of cross-infection while enhancing caregiver safety and convenience, particularly in clinical and long-term care environments. In addition, vital sign data can be transmitted in real time and accessed remotely through secure healthcare platforms, enabling timely clinical assessment and decision-making outside of clinical settings. The ability to support high-frequency and continuous monitoring over extended periods makes contactless monitoring especially well suited for chronic care management, post-acute monitoring, and large-scale health observation scenarios.
Several core technologies enable the practical implementation of contactless vital signs measurement. Each approach differs in sensing principles, measurement accuracy, and suitable for specific applications.
Comparison of Contactless Vital Signs Technologies
| Technology Type | Core Principle | Measured Signals | Strengths | Limitations |
| Image-Based (Camera / rPPG) | Detects subtle skin color changes caused by blood flow | Heart rate, respiratory rate, HRV trends | Low cost, easy deployment, camera-based | Sensitive to lighting and motion |
| Millimeter-Wave Radar | Detects micro chest movements via radio waves | Heart rate, respiration | Works in low light, no camera required | Higher equipment cost |
| Infrared & Thermal Imaging | Measures heat distribution and temperature changes | Respiratory rate, skin temperature | Effective in darkness, contact-free | Lower spatial resolution |
| ToF & Depth Sensing | Uses depth and distance changes over time | Respiratory motion, posture | Robust motion tracking | Requires depth camera integration; Higher hardware costs |
Contactless RPM technologies are now being deployed across a wide range of healthcare and public health environments, including:
Healthcare Facilities: Supports fast, non-invasive assessment without the need to remove clothing or attach sensors.
Elderly and Home Care: Ideal for seniors, people with limited mobility, and chronic disease patients, because it enables safe and accessible monitoring methods at home.
Neonatal / Pediatric Units: Avoid skin irritation from adhesive patches.
Public Health & Pandemic Screening: Supports mass screening while minimizing physical contact.
Data security is a critical requirement for remote patient monitoring (RPM) devices. Modern RPM systems implement multiple layers of protection to safeguard sensitive health information throughout the entire lifecycle. From data collection, transmission, storage, and access, RPM ensures patient privacy and compliance with healthcare regulations.
Most RPM devices encrypt patient data both in transit and at rest, ensuring that physiological data such as vital signs cannot be intercepted or read by unauthorized parties. Secure communication protocols, cloud-based security frameworks, and role-based access controls further limit who can view or manage patient information.
In addition, reputable RPM solutions are developed to comply with major healthcare data protection regulations, such as HIPAA in the United States and GDPR in Europe. These regulatory compliance require strict controls over data privacy, audit logging, and breach prevention.
When properly implemented, remote patient monitoring not only enhances clinical efficiency but also maintains a high level of data integrity, privacy, and cybersecurity, making it a trusted component of modern telehealth and digital care delivery.
Both wearable and contactless vital sign monitoring technologies have distinctive strengths and application scenarios. They are increasingly regarded as complementary rather than competitive. As healthcare continues to evolve toward more flexible and patient-centered models , Contactless Vital Sign Measurement solutions—such as FaceHeart—are expected to play a central role in the next generation of smart health management by enabling frictionless monitoring, multi-environment deployment, and enhanced data privacy.
Below are 5 key advantages of combining RPM with contactless vital sign measurement technologies:
Contactless vital sign measurement removes the need for physical contact, adhesives, and wearable sensors. This approach significantly enhances patient comfort and adherence to monitoring protocols, particularly for elderly patients, pediatric populations, and individuals who require long-term or continuous monitoring.
By eliminating direct skin contact, contactless RPM solutions reduce the risk of cross-contamination. This is especially critical in hospitals, long-term care facilities, and other high-risk clinical environments, where infection control and caregiver safety are critical.
Unlike wearable devices that require user interaction, contactless monitoring enables passive, continuous data collection. Vital signs can be monitored over extended periods without disrupting daily activities or sleep patterns, supporting more natural and reliable long-term observation.
Contactless RPM systems support real-time data transmission of physiological data to secure healthcare platforms. This allows clinicians to access up-to-date physiological data, enabling faster decision-making and proactive intervention.
Without the need to attach physical devices to patients, contactless vital sign measurement can be deployed at scale across a wide range of care settings, including hospitals, long-term care facilities, home care environments, and even public spaces.
Together, these advantages position contactless remote patient monitoring (RPM) as a powerful tool for preventive care, chronic disease management, and the advancement of next-generation digital health solutions.
Further Reading:FaceHeart’s Perspective: Chronic Disease Management with Remote Monitoring
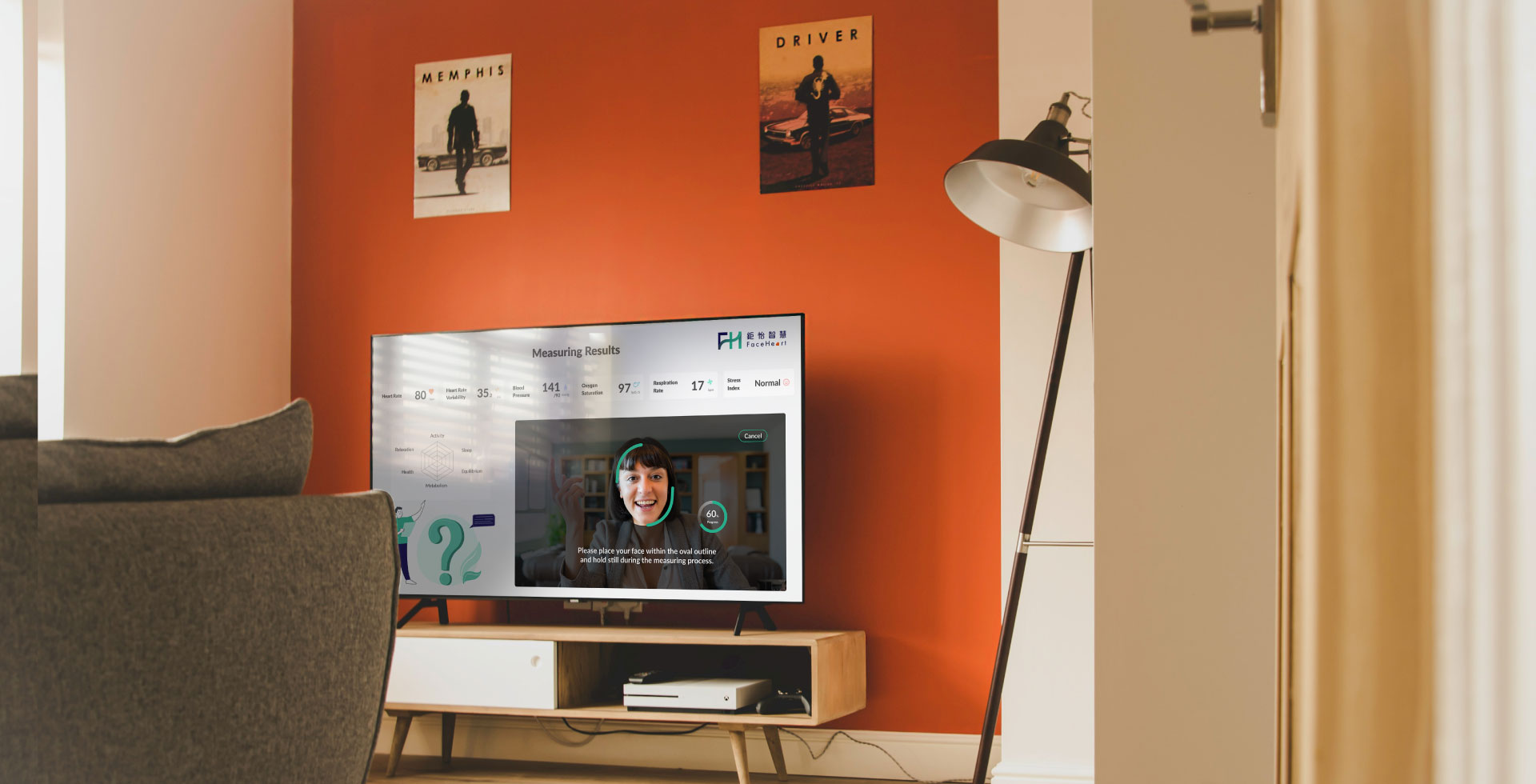
FaceHeart is a global pioneer in Contactless Vital Sign Measurement, offering AI-powered solutions that enable medical-grade monitoring of heart rate, respiratory rate, blood pressure, and blood oxygen, all through everyday cameras on smartphones, tablets, laptops, or smart mirrors.
At the core of the technology is remote photoplethysmography (rPPG), which analyzes subtle facial skin color changes to extract vital sign data. The solution has received FDA 510(k) clearance as a Class II SaMD and is designed with on-device AI processing, ensuring strong data privacy protection. All image data are discarded upon completion.
Beyond hospitals and long-term care facilities, FaceHeart’s contactless monitoring technology is highly scalable for enterprise health management, insurance risk screening, and home wellness monitoring.
Key Breakthroughs of FaceHeart’s Contactless Monitoring Solution:
No specialized hardware is required. Vital signs can be measured via front or rear cameras on smartphones, tablets, or laptops.
Simultaneous tracking of heart rate, respiratory rate, blood pressure, and SpO₂, along with other cardiovascular risks including Cardio Age and CVD Risk
Certified by the U.S. FDA under 510(k) as a medical-grade software.
All processing is done locally on the device, ensuring robust protection of biometric and physiological data.
Designed for seamless integration with clinical systems, elder care platforms, corporate wellness programs, and digital insurance applications.
Fully contactless and comfortable, making it an ideal solution to long-term compliance and user adoption.
For more information on FaceHeart technology, devices, applications, and a live demo, contact [email protected]
Remote patient monitoring solutions enhanced with contactless vital sign measurement technologies are well suited for healthcare and care environments that require long-term monitoring, minimal patient burden, and high scalability. FaceHeart is specifically designed to meet these needs by leveraging image-based, contactless vital sign measurement technology to monitor patients without wearable devices or physical contact. Key application scenarios include:
FaceHeart supports continuous vital sign monitoring in acute and clinical care settings, helping healthcare professionals detect early changes in patient conditions while improving infection control. Its contactless design also reduces the need for device placement and removal, optimizing operational efficiency in high-acuity hospital units.
FaceHeart delivers passive, continuous health monitoring for elderly patients and individuals with chronic conditions. By eliminating the need for wearable devices, it reduces the barrier to adoption and enables care teams to remotely track health trends, identify early changes, and intervene proactively.
Further Reading:Smart Home Health Care: A New Model of Health Technology
The non-invasive nature of FaceHeart makes it well suited for newborns and pediatric populations who are highly sensitive to physical sensors. Reliable physiological data can be obtained without restricting movement or causing discomfort.
FaceHeart’s contactless monitoring capabilities support scalable observation of respiratory patterns and vital signs while minimizing physical interaction. This makes it well suited for environments with high demands for safety, efficiency, and rapid deployment.
The future development of remote patient monitoring (RPM) devices will be driven by the integration of artificial intelligence, contactless sensing technologies, and digital healthcare platforms. Together, these advances are driving RPM beyond basic data collection toward more intelligent, scalable, and proactive care models. Three key directions are defining the next phase of RPM evolution:
Artificial intelligence is transforming remote patient monitoring from passive data collection tools into intelligent, advanced care solutions capable of supporting early risk detection and providing actionable clinical insights. These AI-powered capabilities support more proactive, preventive, and patient-centered care models.
The growing adoption of contactless Vital Sign Measurement significantly reduces reliance on wearable devices while enabling scalable, continuous monitoring across clinical settings, home-based care, and population health programs.
Through enhanced cloud infrastructure and system interoperability, RPM solutions can seamlessly integrate with electronic health records (EHRs), telehealth platforms, and clinical decision support systems, positioning RPM as a core component of next-generation digital healthcare ecosystems.
Overall, these trends position remote patient monitoring as a key pillar of future healthcare systems, supporting value-based care, aging-in-place initiatives, and sustainable care delivery models.
No. Unlike many traditional remote patient monitoring devices that rely on wearables or attached sensors, FaceHeart enables fully contactless monitoring without any wearable devices. By leveraging camera-based rPPG technology, FaceHeart measures vital signs passively, reducing patient burden and improving adherence and long-term monitoring compliance.
Contactless vital sign measurement is not intended to fully replace all traditional medical devices. Instead, it complements existing tools by enabling continuous and remote monitoring. In this case, FaceHeart is particularly effective for trend analysis, early risk detection, and long-term observation on a regular basis or home settings, while conventional devices remain essential in diagnostic confirmation during clinical visits.
Yes. Leveraging advanced signal processing and AI algorithms, such technologies can deliver clinically meaningful results in a fully contactless manner. FaceHeart has obtained FDA clearance in the United States, demonstrating that its technology meets regulatory requirements for safety, performance, and clinical reliability. Designed for home-based and self-managed care environments, FaceHeart provides consistent and repeatable measurements, enabling healthcare professionals to track patient health reliably and make evidence-based clinical decisions.
Remote patient monitoring devices with contactless vital sign measurement are particularly well-suited for elderly individuals, patients with chronic conditions, post-acute care populations, and pediatric or neonatal patients. FaceHeart is designed to support these groups by providing senor-free monitoring, enhancing comfort and reducing barriers to long-term adherence.
In home-based care settings, contactless Vital Sign Measurement enables health monitoring without disrupting daily routines. With FaceHeart, caregivers and clinical teams can remotely track vital sign trends, identify potential abnormalities early, and do so without requiring patients to continuously wear or manage complicated monitoring devices.
For more information on FaceHeart technology, devices, applications, and a live demo, contact [email protected]
Disclaimer: FaceHeart Vitals™ is not intended for diagnostic purposes. If you have any health concerns, please consult your healthcare provider.